Treating Antimicrobial Resistant Infections: A Nano-scale Approach with Big Impacts
Antimicrobial-resistant (AMR) infections are predicted to kill 10 million people each year by 2050—up from 700,000 in 2019—and force 24 million people into extreme poverty as early as 2030. Yet, the pharmaceutical industry has divested from the antibiotic resistance crisis, investing instead in more lucrative types of drugs.

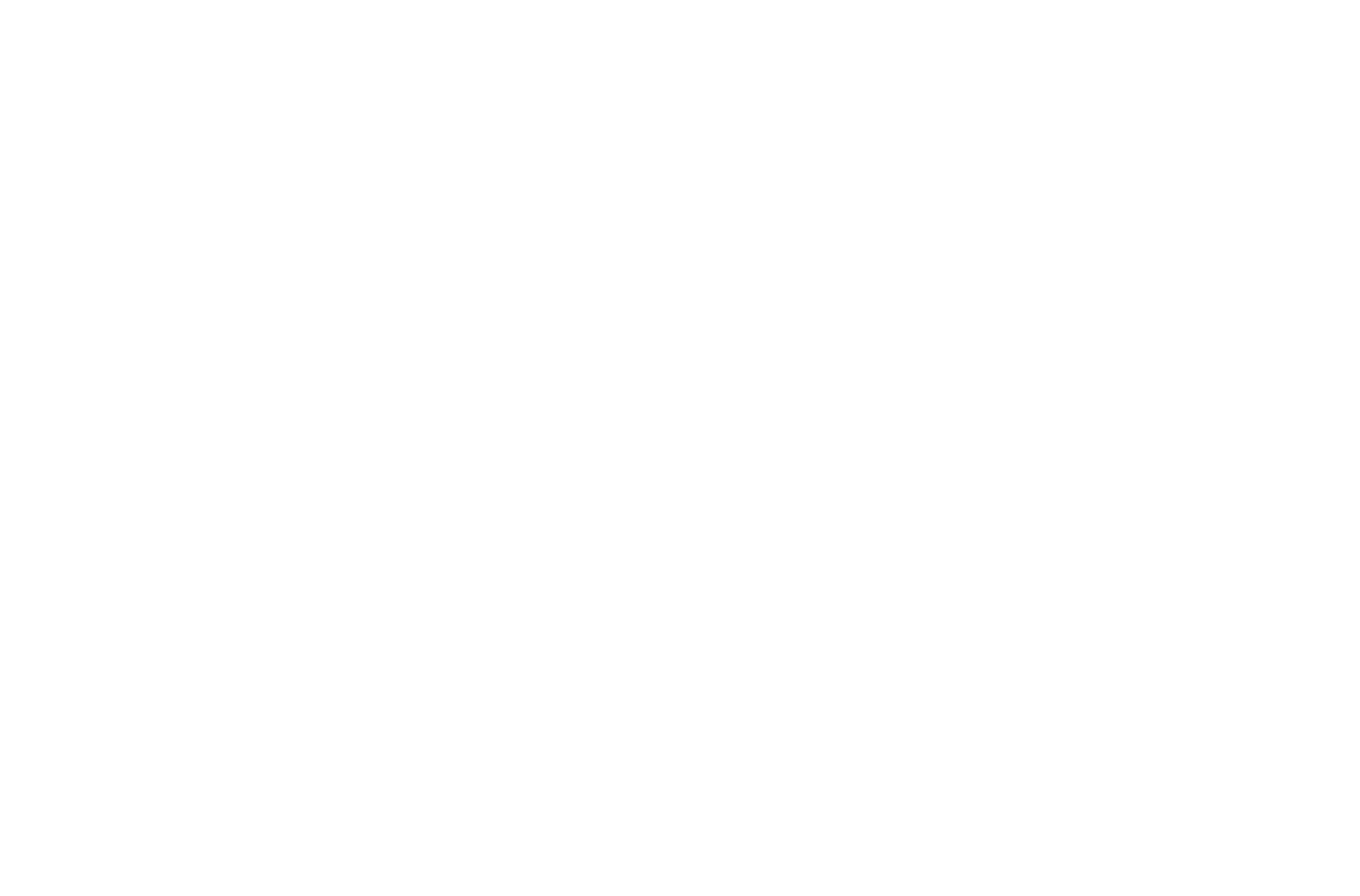
Shaoqin “Sarah” Gong
Increasing AMR and the lack of industry interest have led some research groups to pursue new tools to assist current approaches. One of these methods is nanomedicine, which has been extensively studied for targeted cancer therapy and diagnoses. Nanoparticles, typically smaller than 200 nanometers in diameter, can be used to deliver drugs and treat disease. Professor of Biomedical Engineering at the University of Wisconsin–Madison and the Wisconsin Institute for Discovery Shaoqin Gong’s research group reports an application of nanomedicine to treat antibiotic-resistant pathogens. The study was published in January in Advanced Materials.
The dextran-coated stimuli-responsive nanoparticle Gong’s group developed contains several components that target infected tissue and bacteria both in vitro and in mouse models. Once inside infected tissue, disease-specific stimuli trigger the release of an antibiotic and cationic polymer to eliminate the AMR pathogens.
The hydrophobic core of the nanoparticle, formed by a biodegradable cationic polymer modified with hydrophobic components, can encapsulate FDA-approved antibiotics such as rifampicin. When acting alone, common cationic polymers can kill bacteria, but they can also be toxic to mammalian cells. The polymer used in this nanoparticle, however, is modified with stimuli-responsive linkers that allow the cationic polymer to activate only in the inflammatory microenvironment. The nanoparticle can sense and react to inflammatory responses caused by pathogens, including low pH and high reactive oxygen species (ROS). Once activated, the polymers break down bacterial membranes, allowing rifampicin to enter and kill the bacterium.
This unique stimuli-responsive antibiotic delivery nanoparticle enables us to use FDA-approved drugs that when used alone would not be effective in treating multidrug-resistant bacteria.
In order to target bacteria, the nanoparticle is coated with dextran. Bacterial cell surfaces contain sugar-binding receptors called lectins, for which dextran—a sugar—has a high affinity. Once bound to the bacterial lectins, the nanoparticle destabilizes and releases both cationic polymers and rifampicin. Together, the cationic polymer and antibiotic create a synergistic effect not seen with free rifampicin, which gets rejected by evolved blocking abilities of drug-resistant pathogens.
“This unique stimuli-responsive antibiotic delivery nanoparticle enables us to use FDA-approved drugs that when used alone would not be effective in treating multidrug-resistant bacteria,” Gong says. “By applying this synergy between the stimuli-responsive drug release and the stimuli-responsive cationic polymer, we can treat both gram-negative and gram-positive pathogens. That’s the major impact here.” Gram-negative and gram-positive are classifications of microbes often treated with different antibiotics.
The enhanced permeability and retention effect, a phenomenon where nanoparticles accumulate in certain areas in the body like tumors and infected sites, plays a role in this delivery system as well.
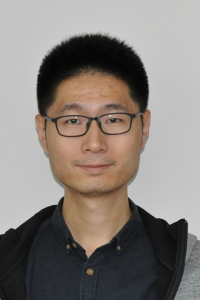
Mingzhou Ye
“Nanoparticles can accumulate in the inflammation site because of the leaky vasculature,” says Mingzhou Ye, lead researcher and postdoctoral associate in Gong’s lab. Once the nanoparticles reach the inflammatory microenvironment and become activated via pH and ROS triggers, “the cationic polymers will agglomerate the bacteria, forming a bacterial cluster including the cationic polymer, the antibiotic, and other nanoparticles that are not fully activated. This cluster contains a high concentration of the polymer and antibiotic so they will have strong antimicrobial efficacy.”
When the antibiotic-bound nanoparticle interacts with the bacteria, there is no stopping it. In vitro, the group found significantly higher efficacy in treating a rifampicin-resistant gram-positive microbe, M. smegmatis, compared to free rifampicin. Notably, no antimicrobial resistance was observed in several generations of nanoparticle-treated E. coli.
Nanomedicine may also be a solution for combatting tough-to-access bugs like slimy buildups of bacteria called biofilms and intracellular infections (bacterial invasion inside host cells), which are difficult to treat with current drug approaches. The Gong lab’s activated nanoparticle was able to penetrate and eliminate P. aeruginosa, E. coli, and MRSA biofilms with much higher efficacy than free rifampicin. In addition, the dextran shell of the nanoparticle can also target infected macrophages and the antibiotic-loaded nanoparticle can be effectively taken up by these immune cells, thereby accessing and killing the intracellular bacteria. Because the cationic polymer can break down rapidly inside the mammalian cell, its biocompatibility is greatly enhanced.
Several in vivo infection models induced by AMR pathogens, including an MRSA thigh infection model, a P. aeruginosa pneumonia model, and an MRSA peritonitis model, showed excellent bacterial targeting ability of the nanoparticle and superior antimicrobial performance. The nanoparticles eliminated more than 99.9% of the pathogens in all the infected organs tested in mice and had a therapeutic efficacy two to three orders of magnitudes higher than free rifampicin. Collaborator David Andes, professor in the Department of Medicine and Department of Medical Microbiology and Immunology, performed the antimicrobial efficacy studies in the P. aeruginosa pneumonia model.
Across all of the methods employed in this study, the active nanoparticle shares a similar outcome: increased efficacy at treating multiple types of bacterial infections compared to an antibiotic alone in drug-resistant pathogens. A single approach to addressing the AMR crisis is unrealistic. “Unless new, effective antibiotics are being developed, we need an alternative approach to tackle this problem,” Gong says. With antimicrobial resistance sharply rising, nanomedicine holds promise.
Author: Martel DenHartog