Sometimes cancer development is not just about a cell having mutations in its DNA, but about when and how those mutations change the cell’s behavior.
UW Carbone Cancer Center member Peter Lewis, PhD, studies how these behavioral changes can lead to cells becoming cancer – and how clinicians and researchers can take advantage of these changes to more effectively target cancers.
In one aspect of his research, Lewis focuses on how genes are turned on and off during embryonic development, and how misregulation in those genes can lead to some childhood cancers.
“In most adult cancers, tumors likely arise from the accumulation of mutations to tumor-suppressing and promoting genes over many years, and in the right context those mutations can lead to cancers,” Lewis said. “But of course children don’t have decades to accumulate mutations, so how do children get tumors early?”

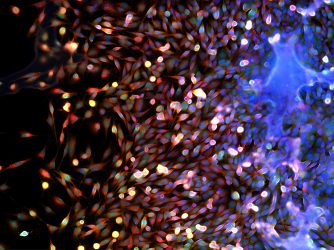
Lewis and his research group at the Wisconsin Institute for Discovery study how mutations in DNA-organizing histone proteins lead to cancer development. For example, in one type of pediatric brain cancer, 85 percent of all tumors have one histone mutation in common. Lewis and his colleagues have shown that, if present at the right time in development, this histone mutation prevents proper gene regulation and causes the stem cells to remain “stuck” in stem cell form, promoting cancer formation. However, if they introduce the mutation into other cells, cancer does not form.
“Most of us get past this window and develop normally, but the children who get these cancers seem to acquire the histone mutation in these specific cell types and in the right developmental window,” Lewis said. “And there are other types of mutations that only work in other specific types of cancer. We don’t know why some cells are exquisitely sensitive to the mutations at specific times, but we do know it’s not a unique problem.”
Lewis’s work has implications not only in pediatric brain cancers, but also in other childhood cancers, in comparing adult to pediatric cancers and in better understanding early human development.
If the histones aren’t there to silence the viruses, then wacky things go on.
In some of those other cancers Lewis referred to, different types of mutations arise not in the histones themselves but in the proteins that deposit histones onto DNA. Still, the end result is similar: genes are turned on or off at the wrong time. In some cases, cancer genes turn on, and these mutations are thus linked to aggressive forms of neuroendocrine tumors, neuroblastomas and leukemias, to name a few. In other cases, however, a different set of genes not necessarily linked to cancer formation turns on.
“Eight percent of our genome are inactive viruses that are inserted in our DNA. They’re inactive because of histone-based silencing mechanisms,” Lewis said. “But if the histones aren’t there to silence the viruses, then wacky things go on.”
Those ‘wacky’ things can lead to viral RNA and protein expression, that can serve as signals to trigger immune surveillance mechanisms. In turn, these mechanism signals to the body’s immune system that something is wrong and the cell needs to be eliminated. Lewis and colleagues, including UW Carbone medical oncologist Josh Lang, MD, think clinicians can exploit this immune response during treatment.
“We’re looking at how we can selectively de-repress these viruses so we can illicit an immune response as a boost to cancer immunotherapy,” Lewis said. “We’re not directly working on the immunotherapy part right now, but we are working on understanding the mechanisms that silence the viral DNA in tumors that might be super-sensitive to perturbations in the silencing pathways.”
This article originally appeared at uwhealth.org.
You must be logged in to post a comment.